PALMETTO STATE EXTRA: Your Health & You!
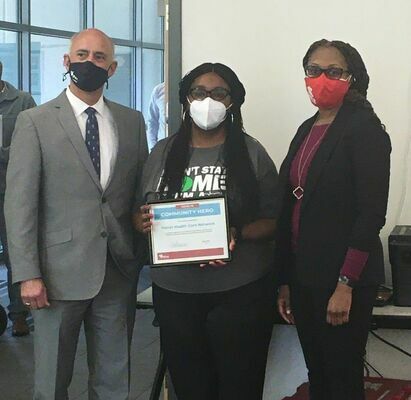 DHEC presents a Community Heroes award to Fetter Health Care Network in Charleston on March 30, 2021. From left to right are Taylor Lee, DHEC’s Lowcountry Regional Health Director; Aretha Powers, Chief Executive Officer for Fetter Health Care Network; and Felicia Veasey, DHEC Community Systems Director for the Lowcountry
DHEC presents a Community Heroes award to Fetter Health Care Network in Charleston on March 30, 2021. From left to right are Taylor Lee, DHEC’s Lowcountry Regional Health Director; Aretha Powers, Chief Executive Officer for Fetter Health Care Network; and Felicia Veasey, DHEC Community Systems Director for the Lowcountry
*Fetter Health Care Network And New Hope Missionary Baptist Church Are The First To Receive New ‘Community Heroes’ Award*
The South Carolina Department of Health and Environmental Control (DHEC) announced Fetter Health Care Network and New Hope Missionary Baptist Church are the first two organizations to be recognized as DHEC’s “Community Heroes in South Carolina.”
The new Community Heroes initiative spotlights local groups and individuals who have helped expand access to COVID-19 education, testing and vaccines throughout South Carolina’s COVID-19 response.
“While DHEC is the state’s lead public health agency, it can’t defeat COVID-19 alone,” said Dr. Edward Simmer, DHEC Director. “DHEC needs help, support, and ideas from community partners to enhance access to education, testing and vaccines in communities across the state. We have many outstanding partners who have sprung into action, and we want to recognize those partners for all of their efforts and to also encourage others to become leaders in their communities.”
Fetter Health
In January, Fetter Health Care Network, a Federally Qualified Health Center in Charleston, vaccinated 580 South Carolina residents at a Baptist church in an underserved area. Fetter worked in close partnership with Royal Missionary Baptist Church in North Charleston to organize and promote the clinic. Fetter has collaborative agreements with multiple churches, schools and organizations in areas where vulnerable populations live, and, in total, Fetter Health has helped administer 16,552 vaccines at 26 sites.
“Success in the fight against COVID-19 will be realized as a group effort,” said Taylor Lee, DHEC’s Lowcountry Regional Health Director. “Fetter Health is a fantastic community resource, and we look forward to continuing to work with them to serve the residents of our great sate. Fetter Health is a true community hero.”
*Understanding How COVID-19 Vaccines Work*
To understand how COVID-19 vaccines work, it helps to first look at how our bodies fight illness. When germs, such as the virus that causes COVID-19, invade our bodies, they attack and multiply. This invasion, called an infection, is what causes illness. Our immune system uses several tools to fight infection. Blood contains red cells, which carry oxygen to tissues and organs, and white or immune cells, which fight infection. Different types of white blood cells fight infection in different ways:
Macrophages are white blood cells that swallow up and digest germs and dead or dying cells. The macrophages leave behind parts of the invading germs, called “antigens”. The body identifies antigens as dangerous and stimulates antibodies to attack them.
B-lymphocytes are defensive white blood cells. They produce antibodies that attack the pieces of the virus left behind by the macrophages.
T-lymphocytes are another type of defensive white blood cell. They attack cells in the body that have already been infected.
The first time a person is infected with the virus that causes COVID-19, it can take several days or weeks for their body to make and use all the germ-fighting tools needed to get over the infection. After the infection, the person’s immune system remembers what it learned about how to protect the body against that disease.
The body keeps a few T-lymphocytes, called “memory cells”, that go into action quickly if the body encounters the same virus again. When the familiar antigens are detected, B-lymphocytes produce antibodies to attack them. Experts are still learning how long these memory cells protect a person against the virus that causes COVID-19.
How COVID-19 Vaccines Work
COVID-19 vaccines help our bodies develop immunity to the virus that causes COVID-19 without us having to get the illness. Different types of vaccines work in different ways to offer protection. But with all types of vaccines, the body is left with a supply of “memory” T-lymphocytes as well as B-lymphocytes that will remember how to fight that virus in the future.
It typically takes a few weeks after vaccination for the body to produce T-lymphocytes and B-lymphocytes. Therefore, it is possible that a person could be infected with the virus that causes COVID-19 just before or just after vaccination and then get sick because the vaccine did not have enough time to provide protection.
Sometimes after vaccination, the process of building immunity can cause symptoms, such as fever. These symptoms are normal and are signs that the body is building immunity.
Types of Vaccines
Currently, there are three main types of COVID-19 vaccines that are authorized and recommended, or undergoing large-scale (Phase 3) clinical trials in the United States. Below is a description of how each type of vaccine prompts our bodies to recognize and protect us from the virus that causes COVID-19. None of these vaccines can give you COVID-19.
mRNA vaccines contain material from the virus that causes COVID-19 that gives our cells instructions for how to make a harmless protein that is unique to the virus. After our cells make copies of the protein, they destroy the genetic material from the vaccine. Our bodies recognize that the protein should not be there and build T-lymphocytes and B-lymphocytes that will remember how to fight the virus that causes COVID-19 if we are infected in the future.
Protein subunit vaccines include harmless pieces (proteins) of the virus that causes COVID-19 instead of the entire germ. Once vaccinated, our bodies recognize that the protein should not be there and build T-lymphocytes and antibodies that will remember how to fight the virus that causes COVID-19 if we are infected in the future.
Vector vaccines contain a modified version of a different virus than the one that causes COVID-19. Inside the shell of the modified virus, there is material from the virus that causes COVID-19. This is called a “viral vector.” Once the viral vector is inside our cells, the genetic material gives cells instructions to make a protein that is unique to the virus that causes COVID-19. Using these instructions, our cells make copies of the protein. This prompts our bodies to build T-lymphocytes and B-lymphocytes that will remember how to fight that virus if we are infected in the future.
Some COVID-19 Vaccines Require More Than One Shot
To be fully vaccinated, you will need two shots of some COVID-19 vaccines.
If you get a COVID-19 vaccine that requires two shots, you are considered fully vaccinated two weeks after your second shot. Pfizer-BioNTech and Moderna COVID-19 vaccines require two shots.
If you get a COVID-19 vaccine that requires one shot, you are considered fully vaccinated two weeks after your shot. Johnson & Johnson’s Janssen COVID-19 vaccine only requires one shot.
If it has been less than two weeks since your shot, or if you still need to get your second shot, you are NOT fully protected. Keep taking all prevention steps until you are fully vaccinated (two weeks after your final shot).
The Bottom Line
Getting vaccinated is one of many steps you can take to protect yourself and others from COVID-19. Protection from COVID-19 is critically important because for some people, COVID-19 can cause severe illness or death.
Stopping a pandemic requires using all the tools available. Vaccines work with your immune system so your body will be ready to fight the virus if you are exposed. After you are fully vaccinated against COVID-19, you may be able to start doing some things that you had stopped doing because of the pandemic. But we’re still learning how vaccines will affect the spread of COVID-19. After you’ve been fully vaccinated against COVID-19, you should keep taking precautions in public places or when you are with unvaccinated people from more than one household.
Getting vaccinated against COVID-19 and following CDC’s recommendations to protect yourself and others will offer the best protection from COVID-19.
*Vaccine Facts If Pregnant Or Breastfeeding*
People who are breastfeeding
Clinical trials for the COVID-19 vaccines currently authorized for use under an Emergency Use Authorization in the United States did not include people who are breastfeeding. Because the vaccines have not been studied on lactating people, there are no data available on:
• The safety of COVID-19 vaccines in lactating people
• The effects of vaccination on the breastfed infant
• The effects on milk production or excretion
The COVID-19 vaccines authorized now are non-replicating vaccines, meaning they are able to create an immune response but do not reproduce inside host cells. Because non-replicating vaccines pose no risk for lactating people or their infants, COVID-19 vaccines are also thought to not be a risk to the breastfeeding infant. Therefore, lactating people may choose to be vaccinated.
People who would like to have a baby
If you are trying to become pregnant now or want to get pregnant in the future, you may receive a COVID-19 vaccine when one is available to you.
There is currently no evidence that any vaccines, including COVID-19 vaccines, cause fertility problems. CDC does not recommend routine pregnancy testing before COVID-19 vaccination. If you are trying to become pregnant, you do not need to avoid pregnancy after receiving a COVID-19 vaccine. Like all vaccines, scientists are studying COVID-19 vaccines carefully for side effects now and will report findings as they become available.
Vaccine side effects
Side effects can occur after receiving any of the available COVID-19 vaccines, especially after the second dose for those that require two doses. Pregnant people have not reported different side effects from non-pregnant people after vaccination with mRNA vaccines (Moderna and Pfizer-BioNTech vaccines). If you experience fever following vaccination you should take acetaminophen because fever has been associated with adverse pregnancy outcomes. Learn more at What to Expect after Getting a COVID-19 Vaccine.
Some people have experienced allergic reactions after receiving a COVID-19 vaccine. Talk with your healthcare provider if you have a history of severe allergic reaction (anaphylaxis) to any other vaccine or injectable therapy (intramuscular, intravenous, or subcutaneous).
Key considerations you can discuss with your healthcare provider include:
The unknown risks of developing a severe allergic reaction
The benefits of vaccination
If you have an allergic reaction after receiving a COVID-19 vaccine during pregnancy, you can receive treatment for it.
Please support The Community Times by subscribing today!
You may also like:







 Loading...
Loading...

